By Sumedha Gupta, IUPUI
CC BY-ND
More than 200 million U.S. residents have gotten at least one shot of a COVID-19 vaccine with the expectation that the vaccines slow virus transmission and save lives.
Researchers know the efficacy of the vaccines from large-scale clinical trials, the gold standard for medical research. The studies found the vaccines to be very effective at preventing severe COVID–19 and especially good at preventing death. But it's important to track any new treatment in the real world as the population-level benefits of vaccines could differ from the efficacy found in clinical trials.
For instance, some people in the U.S. have only been getting the first shot of a two-shot vaccine and are therefore less protected than a fully vaccinated person. Alternatively, vaccinated people are much less likely to transmit COVID-19 to others, including those who are not vaccinated. This could make vaccines more effective at a population level than in the clinical trials.
I am a health economist, and my team and I have been studying the effects of public policy interventions like vaccination have had on the pandemic. We wanted to know how many lives vaccines may have saved due to the states' COVID-19 vaccination campaigns in the U.S.
Building an accurate model
In March 2021, when weekly data on state COVID-19 vaccinations started to become reliably available from state agencies, my team began to analyze the association between state vaccination rates and the subsequent COVID-19 cases and deaths in each state. Our goal was to build a model that was accurate enough to measure the effect of vaccination within the complicated web of factors that influence COVID–19 deaths.
To do this, our model compares COVID-19 incidence in states with high vaccination rates against states with low vaccination rates. As part of the analysis, we controlled for things that influence the spread of the coronavirus, like state–by–state differences in weather and population density, seasonally driven changes in social behavior and non-pharmaceutical interventions like stay-at-home orders, mask mandates and overnight business closures. We also accounted for the fact that there is a delay between when a person is first vaccinated and when their immune system has built up protection.
Vaccines saved lives
To check the strength of our model before playing with variables, we first compared reported deaths with an estimate that our model produced.
When we fed it all of the information available – including vaccination rates – the model calculated that by May 9, 2021, there should have been 569,193 COVID-19 deaths in the U.S. The reported death count by that date was 578,862, less than a 2% difference from our model's prediction.
Equipped with our well-working statistical model, we were then able to “turn off" the vaccination effect and see how much of a difference vaccines made.
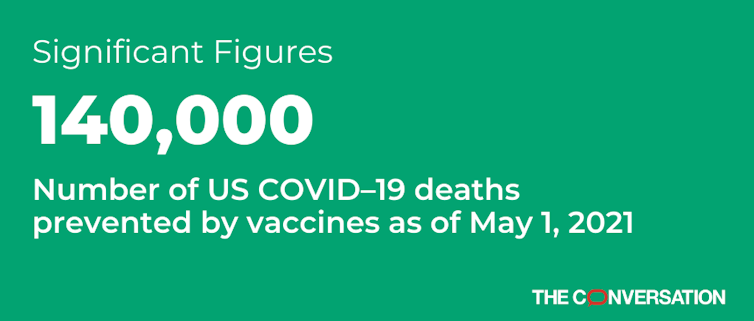
Using near real-time data of state vaccination rates, coronavirus cases and deaths in our model, we found that in the absence of vaccines, 708,586 people would have died by May 9, 2021. We then compared that to our model estimate of deaths with vaccines: 569,193. The difference between those two numbers is just under 140,000. Our model suggests that vaccines saved 140,000 lives by May 9, 2021.
Our study only looked at the few months just after vaccination began. Even in that short time frame, COVID-19 vaccinations saved many thousands of lives despite vaccination rates still being fairly low in several states by the end of our study period. I can say with certainty that vaccines have since then saved many more lives – and will continue to do so as long as the coronavirus is still around.
Sumedha Gupta, Associate Professor of Economics, IUPUI
This article is republished from The Conversation under a Creative Commons license. Read the original article.