Ever since I read the book,
“The Great Influenza: The Story of the Deadliest Pandemic in History" —about the flu epidemic of 1918—I've been worried about another deadly contagion sweeping the planet. So when the the World Health Organization (WHO) declared coronavirus a global public health emergency in January, I was concerned but assumed it would be months before the disease came to my small New Hampshire town. I was wrong.
This past week our rural community confirmed its first case—a male hospital employee who had just returned from a trip to Italy. Ignoring orders to stay at home pending his test results, the man went to a social event, where
he infected at least one other person.
Because coronavirus
spreads with apparent ease from person to person, I imagine it's only a matter of time before the cases in my community start multiplying. I'm a big proponent of yearly flu shots and rigorous handwashing, and I keep antibacterial gel in my car, but I wondered if that's enough to protect myself and my teenage son.
KNOW YOUR RISK FACTORS
This week I spoke with
Brian Yeaman, M.D., a primary care physician in Oklahoma, to better understand how coronavirus differs from regular influenza, and what steps we should be taking to prevent infection.
He told me that coronavirus is similar to influenza in that it's a respiratory virus that spreads through droplets when an infected person coughs or sneezes. As with influenza, those with a compromised immune system or chronic illness are most at risk.
“It's critically important to understand your personal health," Yeaman said. “So if you have diabetes or you have emphysema, that affects your immune system. It's not just if you have an
autoimmune disease."
UNDERSTAND WHAT WE KNOW¬–AND DON'T KNOW–ABOUT THE VIRUS
We don't yet know how long the virus lives on objects such as doorknobs, where it can be spread to the next person. We also don't know the length of the “incubation period"—the time between exposure and the first symptoms (the
WHO's current estimate ranges from 1-14 days)—and to what extent infected individuals can spread the virus when they do not show symptoms.
“Understanding how this virus spreads is the most important thing," Yeaman said, adding that because there has only been limited testing in the U.S., it's difficult to get accurate infection or mortality rates. [On Wednesday, March 4, the Center for Disease Control (CDC) issued
new guidelines expanding testing to any patient with a doctor's order.]
PREVENTION IS COVID-19'S BEST MEDICINE
Testing is only the first step, however. Next comes
treatment.
“With influenza, we have
antiviral medications that work," Yeaman said. “We know that our antiviral meds do not work with coronavirus. That's a significant challenge and the definitive difference."
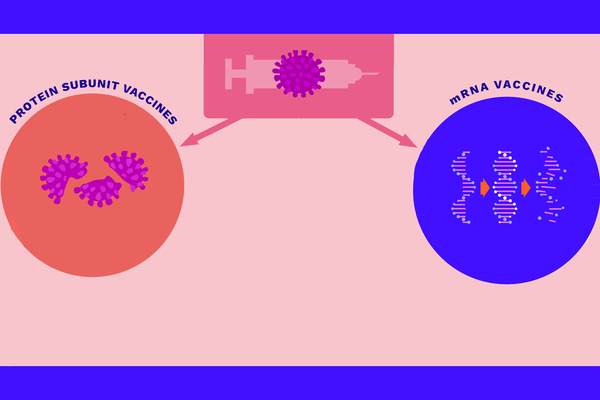
The search for effective treatments and a vaccine are urgently underway around the world, but Anothony Fauci, M.D., the director of the National Institute of Allergy and Infectious Diseases, recently stated that the U.S. is still
12 to 18 months from developing a vaccine.
Given the current lack of definitive treatment or vaccine, experts including Dr. Yeaman recommend taking
preventative measures, such as regular hand-washing, not touching one's face, using hand sanitizer after touching surfaces, and staying at least three feet away from anyone who is coughing or sneezing.
For those who are sick, it's vitally important to protect others by coughing into your arm or a tissue, regularly cleaning your hands and, above all, staying home. I wish the patient in my community had followed this last protocol.
PROTECTING NEW MOTHERS AND BABIES
As a reasonably healthy woman in my 50s, I'm not overly concerned about getting seriously ill, even if I contract the virus. But I do worry about more vulnerable populations, like pregnant women. I reached out to
Rashmi Kudesia, M.D., a reproductive endocrinologist and infertility specialist in Texas and a member of HealthyWomen's Women's Health Advisory Council.
In an email exchange, Kudesia told me that there isn't enough data to quantify the threat to pregnant women and nursing mothers. “However, as with other coronaviruses that have become pandemic in the past, such as
SARS and MERS, it seems reasonable to assume that as pregnancy suppresses the immune system, pregnant women are at higher risk for severe illness," wrote Dr. Kudesia. She added that there is some data to suggest an increased risk of obstetric complications, such as preterm birth.
>It's important to note that Dr. Kudesia said that
influenza remains a far greater threat to pregnant women and nursing mothers.
“Pregnant women take up an outsized proportion of influenza-related deaths each year, mostly among women who have declined vaccination," she wrote. “Of course, our knowledge of COVID-19 is still developing, but thus far, it is far more likely that a pregnant or nursing mother in the U.S. would be exposed to or face complications from influenza than COVID-19."
Kudesia explained that the main concern for infected nursing mothers is spreading the virus to their child via airborne respiratory droplets, rather than via breast milk.
“Nursing mothers may consider wearing a mask while nursing, or having another healthy parent or adult feed the child using expressed breast milk," wrote Kudesia, citing the
CDC guidelines.
VIDEO CHATTING WITH GRANDPARENTS, QUARANTINING WITH KIDS
Aside from pregnant women, another vulnerable population is
seniors, who have contracted the virus in far greater numbers than children. Yeaman explained that our immune system shifts at age 65 and is compromised, by definition, at age 80. For this reason (and the fact that kids are constantly touching their faces and may not have the cleanest hands) he recommends seniors avoid contact with small children.
“You don't want to lose touch with your grandkids, but some isolation right now in terms of physical contact wouldn't be the worst idea," Yeaman said, adding that video chats can be a safer alternative.
As it happens, we have two senior communities near our elementary and middle schools.
Despite the two confirmed cases in our town, the schools remain open, but this past week the high school cancelled overseas service trips due to fears about the virus. I know of a few families who scrambled to make alternative plans for their kids.
At least high schoolers can stay home alone. For families with young children, school closures could prove a real challenge, particularly for working parents.
Meg Darrow Williams, a preschool teacher and mother of two children ages 8 and 13 in our community told me she's personally nervous but trying to remain calm.
“I'm in a high-risk category because I'm immunosuppressed," Williams said. “I'm staying informed by speaking with my doctor and I only get my information from reputable sources, such as the CDC."
Williams has stocked up on frozen food and supplies, but feels ambivalent about doing so. “I've seen photos of empty supermarket shelves and didn't want to look that nervous, but at the same time I want to be smart."
She tells me if the schools close, she'll stay home with her kids, adding that many of the teachers at her preschool are also parents.
“I imagine it might eventually have a domino effect. My husband will continue to go to work as long as he's able," Williams said.
I'm lucky that no one in my family is in a high-risk category, my kids are older (I have a daughter in college) and I work from home. My son and I have discussed the possibility of having to quarantine in our house and his school is already set up to assign work remotely online.
Despite the fact that a vaccine is a year or more away, I'm not panicking. Now all I need is for my local CVS to get more hand sanitizer.
For most recent updates on coronavirus:
World Health Organization
Centers for Disease Control and Prevention (CDC) Information on COVID-19 and Pregnant Women and Children
Centers for Disease Control and Prevention (CDC) Information on COVID-19 and Resources for Households
Centers for Disease Control and Prevention (CDC) Information on COVID-19